Cardiac surgery, or cardiovascular surgery, is surgery on the heart or great vessels performed by cardiac surgeons. Continually, it is done to treat complications of ischemic heart disease (for example, coronary artery bypass grafting), correct congenital heart disease, or treat valvular heart disease from various causes including endocarditis, rheumatic heart disease and atherosclerosis. It also includes heart transplantation.
Coronary Artery Bypass Graft Surgery (CABG)
What is coronary artery disease?
The heart is basically a pump. The heart is made up of specialized muscle tissue, called the myocardium. The heart's primary function is to pump blood throughout the body, so that the body's tissues can receive oxygen and nutrients.
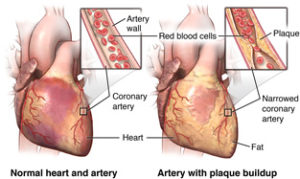
Like any pump, the heart requires fuel in order to work. The myocardium requires oxygen and nutrients, just like any other tissue in the body. However, the blood that passes through the heart's chambers is only passing through on its trip through the body. This blood does not give oxygen and nutrients to the myocardium. The myocardium receives its oxygen and nutrients from the coronary arteries. The coronary arteries lie on the outside of the heart and supply oxygenated blood to the heart tissue.
Coronary artery disease (CAD) is the narrowing of the coronary arteries (the blood vessels that supply oxygen and nutrients to the heart muscle), caused by a buildup of fatty material within the walls of the arteries. This buildup causes the inside of the arteries to become narrowed, limiting the supply of oxygen-rich blood to the heart muscle.
When the heart tissue does not receive an adequate blood supply, it cannot function as well as it should. If the myocardium's blood supply is decreased for a length of time, a condition called ischemia may develop. Ischemia can decrease the heart's pumping ability, because the heart muscle is weakened due to a lack of oxygen.
What are the symptoms of Coronary Artery Disease?
Symptoms of coronary artery disease may include, but are not limited to, the following :-
Unfortunately, there may be no symptoms of early coronary artery disease, yet the disease will continue to progress until sufficient artery blockage exists to cause symptoms and problems. If the blood supply to the heart muscle continues to decrease as a result of increasing obstruction of a coronary artery, a myocardial infarction, or heart attack, may occur. If the blood flow cannot be restored to the particular area of the heart muscle affected, the tissue dies. And the heart weakens for ever and can not be repaired, so before the artery gets blocked the block has to be bypassed.
What are the methods used for CABG surgery?
Coronary artery bypass surgery is performed to treat a blockage or narrowing of one or more of the coronary arteries, thus restoring the blood supply to the heart muscle.
1. Conventional or On Pump CABG
In this method chest is opened (breastbone (sternum) is cut in half and spread apart) heart is exposed, tubes are inserted into the heart so that the blood can be pumped through the body during the surgery by a cardiopulmonary bypass machine (heart-lung machine). and then heart is stopped for some time so that the surgeon can perform the bypass. During this period “Bypass machine” is necessary to circulate blood in whole of the body, after surgeon to performs the bypass operation the heart is restarted by giving some medicines, as the heart starts beating again, the blood circulation is again shifted by gradually loading heart from pump to heart.
2. Off-pump" CABG or “beating heart bypass”
While the traditional "open heart" procedure is still performed and often preferred in many institutions, newer less invasive techniques have been developed to bypass blocked coronary arteries. "Off-pump" procedures or “beating heart bypass” , in which the heart does not have to be stopped, was developed in the late 1990's. The part of the heart is stabilized using the device called “Octopus stabilizer”, and then the surgery is done on that part of heart. This is a better procedure and the recovery is much faster than conventional bypass surgery.
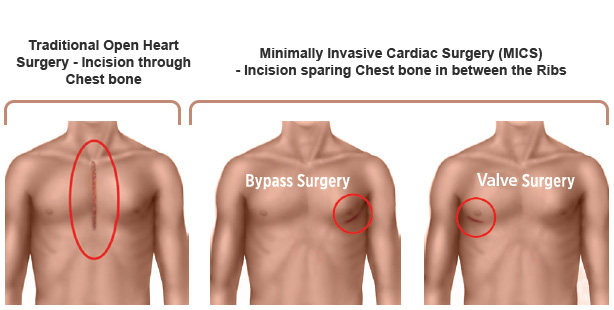
3. M.I.C.S. CABG
Minimally-invasive procedures, such as key-hole surgery (performed through very small incisions) is increasingly being used. In this the operative procedure is same but the approach to heart is changed , only 7 to 9 cm long incision is made in the lower chest and whole of sternum need not be cut across. This carries less bleeding risk, less pain etc. and faster recovery is possible. All newer techniques are preferred because they alter the body homeostasis minimally and thus the recovery is faster, complications are less.
4. What is Awake Non Intubated CABG?
When the patient is having renal or lung diseases along with cardiac problem, and the patient is not fit for the general anesthesia and there is fear of ventilator dependence after surgery, this is the procedure adopted. In this type of bypass surgery , the procedure is done on beating heart or some times conventional bypass and the patient’s upper chest is made numb by putting a small catheter in the back near the spinal cord . As the chest is numb the patient does not feel pain of surgery and whole of bypass surgery is done without making patient unconcious , and only mild sedation is given. During whole procedure patient breathes of his own even patient can continue to talk to the surgeon during surgery.
This procedure is very useful for asthma patients whom we fear that after surgery they may not come out of ventilator .
What are the grafts or conduits used for bypass surgery?
Blood vessels, or grafts, used for the bypass procedure may be
One end of the graft is attached on the aorta and the other end is attached below the blockage. Thus, the blood is rerouted around, or bypasses, the blockage through the new graft to reach the heart muscle.
What are the benefits of Arterial Grafts?
These are the arteries preferably IMA (Internal MAMMARY Artery) from inside of chest, Radial arteries from wrist etc. as they are arteries they remain patent for a longer period and the patency period is as long as 20 yrs. So they are preferred grafts for patients in their 50s and 60s. Also for those who don’t prefer to have long incisions in their legs.
How much is the risk of CABG?
CABG is a standardized procedure now, it carries a risk of less than 1% ( Low risk Category patients) to 3% ( high Risk category patients) chance of death in 30 days post op. in view of disease profile , as it usually is associated with many comorbid conditions ( Diabetes, Lung disease due to smoking, obesity, old age etc) this is considered to be low risk procedure. Though wound infesctions, cough, bleeding, stroke etc are some other complications can happen. But overall looking at the complexity and risk of disease profile this can be considered as negligible risk.
How could be life style after CABG?
Post surgery mostly by 6 weeks the patient returns to routine life style. They can be allowed to do regular and moderate heavy works after 3 months and proper heavy works after 6 months. All other functional details are there in REHAB section please go through them.
Mitral Valve Replacement Surgery
Surgery may be necessary when the valve opens or closes incompletely. A stenotic (narrow) valve does not let the blood easily into the heart pumping chamber (Left Ventricle), causing blood to "back up" and pressure to build up in the lungs. This makes it difficult for the heart to increase the amount of blood that it pumps with exercise, and may produce symptoms of shortness of breath - especially with activity. And also the congested lungs don’t allow air to be filled in the lungs and so pt feels difficulty in breathing while lying down.
If the leaflets do not meet correctly for any reason (and many things may cause this), blood may leak backward into the lungs each time the heart pumps. Since some of the blood leaks backwards, the heart has to pump more blood with each contraction in order to push the same amount of blood forward. This is called volume overload. The heart can compensate for this overload for many months or years, provided that the leakage came on slowly and progressively. Eventually, the heart begins to fail and patients show symptoms of shortness of breath or fatigue (tiredness).
What causes mitral valve problems?
Most intact aortic aneurysms do not produce symptoms. As they enlarge, symptoms such as abdominal painand back pain may develop. Compression of nerve roots may cause leg pain or numbness. Untreated, aneurysms tend to become progressively larger, although the rate of enlargement is unpredictable for any individual. Rarely, clotted blood which lines most aortic aneurysms can break off and result in an embolus.
What are the surgical options?
Many mitral valves can be repaired, especially if they leak due to degenerative disease. A separate discussion of mitral valve repair will be available through this site. In many cases, however, the valve is too damaged to permit repair and the valve must be replaced with a prosthetic (artificial) valve. Valves damaged by rheumatic disease often must be replaced. In general terms, there are two types of artificial valves available - mechanical valves made entirely from metal and pyrolytic carbon - or biological valves - made from animal tissues. Each has advantages and disadvantages with respect to durability (how long they will last) and risk of blood clots forming on the valve. The choice of which type to use should be made by you and your doctors taking the following into consideration:
Examples of the valves that your cardiothoracic surgeon might use are pictured below.
Mechanical valves
There are a number of excellent mechanical prostheses available today. All perform equally well. The principle advantage of mechanical valves is their excellent durability. The valves available today simply do not wear out! Their main disadvantage is that blood has a tendency to clot on all mechanical valves. If this happens the valve will not function normally. Therefore, patients with these valves must take anticoagulants (blood thinners) for life. There is also a small but definite risk of blood clots causing stroke, even when taking anticoagulants.
Biological valves
There are a variety of biological alternatives for mitral valve replacement. Most are made from cow or pig tissue. Their key advantage is that they have a reduced or no risk of blood clots forming on the valve itself causing valve dysfunction or stroke. The key disadvantage of biological or tissue valves is that they have more limited durability as compared with mechanical valves. They will wear out given enough time. The rate at which they wear out, however, depends on the patient's age. A young boy might wear out such a valve in only a few years, while the same valve might last 10-15 years in a middle aged person, and even longer in a patient over the age of 70. Of course, as we grow older we expect that we will not need the valve for as many years as our life expectancy is less. The general consensus is that a tissue valve may not need to be replaced if used in a patient over the age of 55-70 years. However with newer bioprosthetic pericardial valves the durability is better and they can be implanted in pts as young as 45 yr.
What are the risks of surgery?
After successful mitral valve replacement you can expect to return to your preoperative condition or better, although this may take time. Anticoagulation (blood thinners) with Coumadin is often prescribed for 6 weeks to 3 months postoperatively for those with biological valves, and for whole life for those with mechanical valves. Once your wounds have healed there should be few, if any, restrictions on your activity.
Aortic Valve Replacement Surgery
What is aortic valve disease?
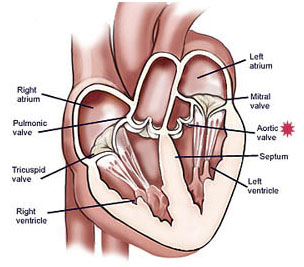
There are four valves in your heart including the mitral, tricuspid, aortic and pulmonic valves.
The aortic valve is located between the left ventricle (lower heart pumping chamber) and the aorta, which is the largest artery in the body. Valves maintain one-way blood flow through the heart.
What is the aortic valve?
What is the aortic valve?
There are four valves in your heart including the mitral, tricuspid, aortic and pulmonic valves.
The aortic valve is located between the left ventricle (lower heart pumping chamber) and the aorta, which is the largest artery in the body. Valves maintain one-way blood flow through the heart.
What is aortic valve disease?
Aortic valve disease occurs when the aortic valve does not work correctly. This can be caused by:
What causes aortic valve disease?
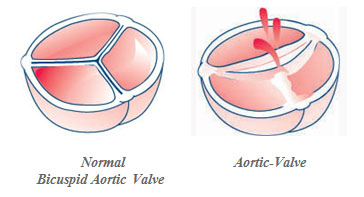
The aortic valve may be abnormal at birth (typically a bicuspid congenital aortic valve) or become diseased over time, usually seen in older patients (acquired valve disease).
Congenital aortic valve disease
Patients with bicuspid aortic valves are born with them and are present in about 1 - 2 percent of the population.
Instead of the normal three leaflets or cusps, the bicuspid aortic valve has only two. Without the third leaflet, the valve opening may not close completely and leak (regurgitant) or not open completely and become narrowed (stenotic) or leak.
In many cases, bicuspid aortic valves may function normally for several years without requiring treatment.
About 25 percent of patients with bicuspid aortic valves may have some enlargement of the aorta above the valve. If it is greatly dilated, the aorta is known as being aneurismal.
Acquired aortic valve disease
With acquired aortic valve conditions, changes occur in the structure of the valve. Acquired aortic valve conditions include:
What are the symptoms of aortic valve disease?
Many patients with aortic valve disease are asymptomatic (have no symptoms), even when the stenosis (narrowing) or insufficiency (leak) are severe.
Initial symptoms of aortic valve disease usually include:
More advanced symptoms may include:
How is aortic valve disease treated?
If you do not have symptoms or heart damage, you will need to protect your valve from further damage. Where as those patients who are having symptoms can be treated with medicines initially but when the symptoms get worse or the echo shows that the heart is getting weak then surgical interventions are done.
Aortic valve surgery
There are two types of aortic valve surgery: aortic valve repair and aortic valve replacement.
During aortic valve surgery, including aorta surgery, the aortic valve may be repaired or replaced. The results of your diagnostic tests, the structure of your heart, your age, the presence of other medical conditions and other factors will be considered to determine whether aortic valve repair or replacement is the best treatment approach for you.
Aortic valve surgery can be performed using traditional heart valve surgery or minimally invasive approaches.
Traditional Aortic Valve Surgery
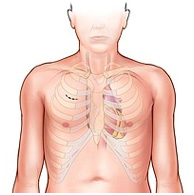
During traditional aortic valve surgery, a surgeon makes a 6- to 8-inch incision down the center of your sternum, and part or all of the sternum (breastbone) is divided to provide direct access to your heart. The surgeon then repairs or replaces your abnormal heart valve or valves.
Minimally Invasive Aortic Valve Surgery
Minimally invasive aortic valve surgery is a type of aortic valve repair surgery performed through smaller, 2- to 4-inch incisions without opening your whole chest. This is typically done with a “J” incision and leaves your chest stable. Minimally invasive surgery reduces blood loss, trauma, length of hospital stay and may accelerate recovery. Most patients who require isolated aortic valve surgery are candidates for minimally invasive aortic valve surgery, but your surgeon will review your diagnostic tests and determine if you are a candidate for this type of surgery.
Aortic valve repair
While the aortic valve is usually replaced, aortic valve repair may be an option. (Details of Aortic valve repair is there in next segment)
Repair of an enlarged aorta
Aortic valve disease is often associated with enlargement (aneurysm) of the ascending aorta, the initial portion of the aorta (the main blood vessel in the body that originates from the aortic valve).
If the enlargement of the aorta is substantial (usually above 4.5 or 5 cm in diameter), this part of the aorta may need to be replaced. The replacement is done at the time of aortic valve repair or replacement.
Repair of valve tears or holes
In addition, if the valve leaflets have tears or holes, the surgeon can patch these with tissue patches.
Aortic valve replacement
If valve repair is not an option, your surgeon may replace the valve. The native (original) valve is removed and a new valve is sewn to the annulus of your native valve. The new valve can either be mechanical or biological.
Biological valve replacement
Biological valves (also called tissue or bioprosthetic valves) are made of tissue, but they may also have some artificial parts to provide additional support and allow the valve to be sewn in place.
Biological valves can be made from pig tissue (porcine), cow tissue pericardial (bovine), or pericardial tissue from other species.
These valves are safe to insert, durable (lasting from 15 to 20 years), and allow patients to avoid lifetime use of anticoagulants (blood thinning medications). As in India mostly diagnostic facilities for estimation of blood thinning are not widespread and older patients are not medically insured and dependent on family, maintenance of anticoagulation is difficult. So mostly patients should be offered this biological valve.
Mechanical valves replacement
Mechanical valves are made completely of mechanical parts, which are non-reactive and tolerated well by the body. The bileaflet valve is used most often.
It consists of two pyrolite (qualities similar to a diamond) carbon leaflets in a ring covered with polyester knit fabric.
All patients with mechanical valve prostheses need to take an anticoagulant medication, warfarin (Coumadin), for the rest of their life to reduce the risk of blood clotting and stroke. This increases the risk of bleeding.
This is offered to the patients of age less than 40 years, as they have to live long and biological valve implantation in them will need resurgery once or twice.
What is the risk of aortic valve surgery?
The overall risk of death associated with surgery for isolated aortic valve replacement is less than 1%, In cases of Severe Calcific Aortic valve disease the chances of conduction block is there in which case the patient may require pacemaker implantation .
Mitral Valve Repair Surgery
Advantages of Valve Repair: Why Repair Is Better Than Replacement
Valve repair is the best option for nearly all patients with a leaking (regurgitantl valve and for many with a narrowed (stenotic) valve.
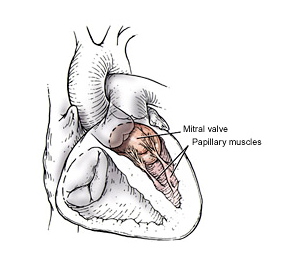
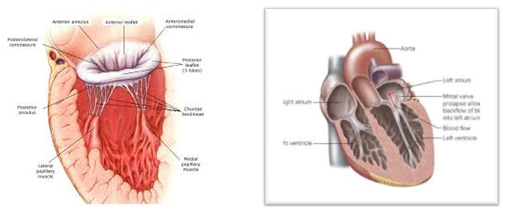
Mitral Valve
This valve protects the back flow of pumping left ventricular blod to Left Atrium and thus the lungs. When this valve gets diseased leaking ir narrowing the blood pressure in lungs increase and the patient starts getting features of easy fatigusbility, difficulty in breathing, coughing while sleeping and lying down, and recurrent chest infections and weight loss.
Techniques of Mitral Valve repairs
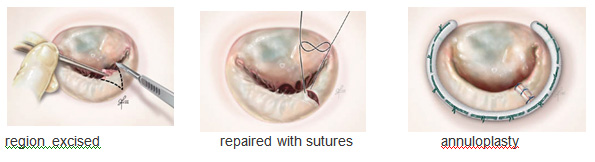
Mitral Valve Posterior Leaflet Prolapse — Valve Repair Surgery
During mitral valve repair heart surgery, triangular resection is the technique used most frequently for posterior leaflet prolapsed.
Triangular Resection Mitral Valve Repair
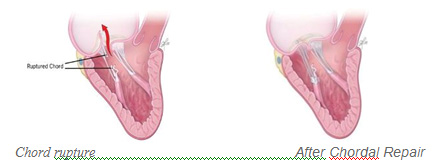
Mitral Valve Anterior Leaflet Prolapse — Valve Repair Surgery
When there is mitral valve prolapse of the anterior leaflet, repair is more complex and requires greater surgical expertise. To correct anterior leaflet prolapse caused by a ruptured or elongated chord, we usually create new chords out of Goretex. These Goretex chords generally last forever.
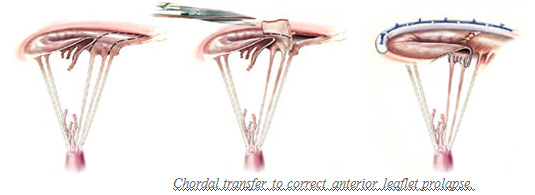
A second technique used for correction of anterior leaflet prolapse is chordal transfer, which involves transfer of chords from another part of the valve to the area with abnormal chords. Both techniques provide excellent long-term results for patients. Long-term durability is excellent. The new chordae do not rupture or elongate.
Chordal Transfer to Treat Anterior Leaflet Prolapse
Posterior leaflet chordae are transferred to the unsupported free edge of the anterior leaflet. The posterior leaflet is then repaired. A cloth annuloplasty band completes the repair.
Comissurotomy
When the leaflets are leaking due to the abnormal adhesions between the leaflets making them lesser mobile thus causing them to leak, so during surgery the adhesion on the commisures are lysed by sharp dissection with knife making the leaflets free and mobile.
All repairs include an annuloplasty, which is a complete or partial ring placed aroundthe circumference (rim) of the valve.
Almost all the rheumatic valves are thickened due to the inflammatory process, which makes the leaflet less mobile and stiff. By Peeling of the leaflet fibrotic tissues the leaflets are made pliable and thus are better in functionality.
Aortic Valve Repair Surgery
This valve protects the leakage of blood from the Aorta back to the heart after its been pumped from Left Ventricle. When this valve is leaking or narrowed it causes low effective blood pumping to body.
So patients complain of recurrent vertigo or chakkar, Episodes of unconsciousness, and easy fatiguability.
Technique of aortic valve repair
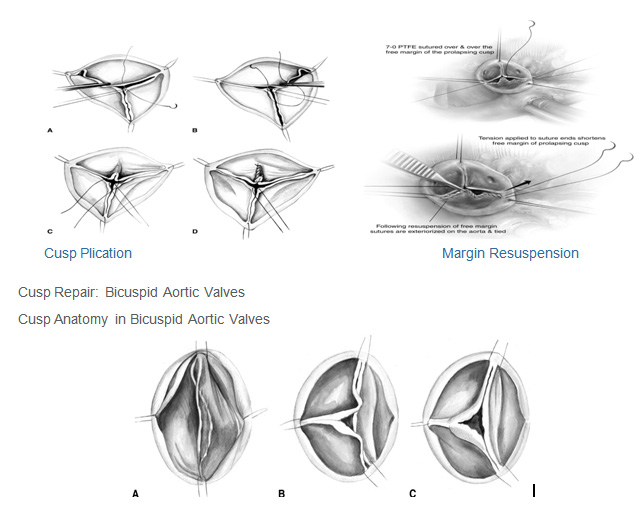
Cusp Repair: Tricuspid Aortic Valves
Cusp prolapse is associated with excess length of the free margin, which can be corrected using either central free margin plication or free margin resuspension.
Free Margin Plication
Bicuspid aortic valve disease affects not only the valve cusps but also the functional aortic annulus. Bicuspid AV may be divided into two general types.
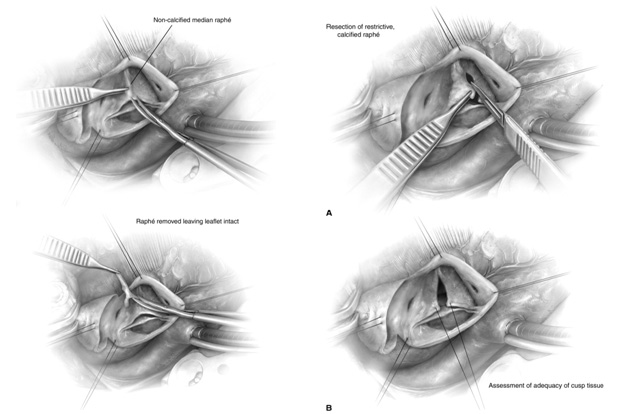
Type 1 Valve: Raphé Shaving and Preservation
Type 1 Valve: Management of a Restrictive or Calcified Raphé
Congenital Heart Disease Surgery
VSD
What is it?
VSD is a hole in the wall separating the two pumping chambers of the heart.
In normal development, the wall between the chambers closes before the fetus is born, so that by birth, oxygen-rich blood is prevented from mixing with the unoxygened dirty blood. When the hole does not close, it may cause higher pressure in the heart and lungs along with reduced oxygen to the body.
How does it affect the heart?
Normally, the left side of the heart only pumps blood to the body, and the heart's right side only pumps blood to the lungs. In a child with VSD, blood can travel across the hole from the left pumping chamber (left ventricle) to the right pumping chamber (right ventricle) and out into the lung arteries. If the VSD is large, the extra blood being pumped into the lung arteries makes the heart and lungs work harder and the lungs can become congested.
How does the VSD affect my child?
If the opening is small, it won't cause symptoms because the heart and lungs don't have to work harder. The only abnormal finding is a loud murmur (noise heard with a stethoscope).
If the opening is large, the child may breathe faster and harder than normal. Infants may have trouble feeding and growing at a normal rate. Symptoms may not occur until several weeks after birth. High pressure may occur in the blood vessels in the lungs because more blood than normal is being pumped there. And this congestion leads to repeated lung infection. Over time this may cause permanent damage to the lung blood vessels.
What happens if VSD is not closed
The continuous leakage of blood at pressure from left chamber to right chamber leads to high blood pressure in the lungs. This can make the arteries of lungs stiff, which eventually gets dependent on high pressure. In such situation hole closure may cause heart and lung failure. That means delay in VSD closure make the disease inoperable. And patient becomes crippled due to decreased oxygenation of blood , this situation is called “Eisenmingerisation” . such patients do not live long , remain on oxygen and bed ridden. So it is advisable to get it operated in time as this disease is completely curable.
What can be done about the VSD?
If the opening is small, it won't make the heart and lungs work harder. Surgery and other treatments may not be needed. Small VSDs often close on their own. There isn't any medicine or other treatment that will make the VSD get smaller or close any faster than it might do naturally.
If the opening is large, open-heart surgery may be needed to close it and prevent serious problems. Babies with VSD may develop severe symptoms and early repair, within the first few months, is often necessary. The repair may be delayed in other babies. Medicines may be used temporarily to help with symptoms, but they don't cure the VSD or prevent permanent damage to the lung arteries.
Closing a large VSD by open-heart surgery usually is done in infancy or childhood even in patients with few symptoms, to prevent complications later. Usually a patch of fabric or pericardium (the normal lining around the outside of the heart) is sewn over the VSD to close it completely. Later this patch is covered by the normal heart lining tissue and becomes a permanent part of the heart.
If an infant is very ill, or has more than one VSD or a VSD in an unusual location, a temporary operation to relieve symptoms and high pressure in the lungs may be needed. This procedure (pulmonary artery banding) narrows the pulmonary artery to reduce the blood flow to the lungs. When the child is older, an operation is done to remove the band and fix the VSD with open-heart surgery.
What the child need in the future?
The cardiologist will make sure that the heart is working normally. The long-term outlook is good and usually no medicines or additional surgery are needed.
What if the defect is still present? Should it be repaired in adulthood?
Usually closure is recommended for small VSDs only if there's been an episode of endocarditis which is a heart infection that may be due to the VSD, or if the location of the VSD affects the function of one of the heart valves.
If the VSD is large, the pressure in the lungs determines whether it can be closed in an adult patient. Those with low lung pressures will benefit from surgery; those with high pressures may or may not.
Medical Follow-up
A cardiologist should examine you regularly. If your VSD is small or was closed as a child and no other problems are detected, visits every 3–5 years are probably sufficient.
Activity Restrictions
Most patients won't need to limit their activity. However, if you have pulmonary hypertension or your heart doesn't pump as well as it used to, you may need to limit your activity to your endurance. Your cardiologist will help determine if you need to limit your activity.
Pregnancy
Once the VSD is closed and there's no leftover pulmonary hypertension, the risk from pregnancy is low. If the VSD stays open, it will be necessary to talk to your cardiologist. Unless pulmonary hypertension is present, pregnancy may be well tolerated, but before you decide to get pregnant you need to find out the exact risks to you and your child. See the sections on Pregnancy and Genetic Counseling for more information.
Will You Need More Surgery?
People whose ventricular septal defects are repaired rarely need more surgery unless the patch leaks or other holes are discovered later. If this occurs, whether you'll need surgery depends on the size of the residual defects.
T.O.F. (TETRALOGY OF FALLOT’s)
It is the most common cyanotic heart defect, and the most common cause of blue baby syndrome.
TOF is treated with corrective surgery, usually within the first year of life, but presents with a long-term problems including arrhythmia, pulmonary regurgitation, and re-operation.
Discription of disease
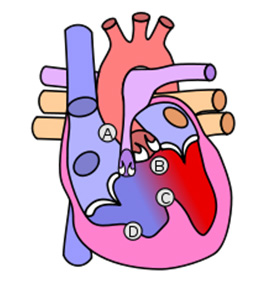
As such, by definition, Tetralogy of Fallot involves four heart malformations which present together:
A:Pulmonary Infundibular Stenosis : A narrowing of the right ventricular outflow tract. It can occur at the pulmonary valve (valvular stenosis) or outflow tract due to overgrowth of the heart muscle wall. This causes reduced blood flow to the lungs and thus the oxygenation of blood reduces.
B:Overriding Aorta The aorta which supplies blood to whole body is situated just above the hole in heart (VSD) and hence draws both pure and impure blood (biventricular connection), as it is connected to both the right and the left ventricle. The degree to which the aorta is attached to the right ventricle is referred to as its degree of "override." The degree of override is extremely variable, with 5-95% of the valve being connected to the right ventricle.
C:ventricular septal defect(VSD) A hole between the two pumping chambers (ventricles) of the heart and in the majority of cases is single and large. This causes mixing of pure and impure blood.
D: Right ventricular hypertrophy The right ventricle is more muscular than normal, causing a characteristic boot-shaped (coeur-en-sabot) appearance as seen by chest X-ray. the right ventricular wall increases in size to deal with the increased obstruction to the right outflow tract.
How do we recognize?
Digital clubbing with cyanotic nail beds in an adult with tetralogy of Fallot.
Tetralogy of Fallot results in low oxygenation of blood due to the mixing of oxygenated and deoxygenated blood in the left ventricle via the ventricular septal defect (VSD) and preferential flow of the mixed blood from both ventricles through the aorta because of the obstruction to flow through the pulmonary valve. This is known as a right-to-left shunt.
1.The primary symptom is low blood oxygen saturation with or without cyanosis (blue discoloration of nails, lips and skin) from birth or developing in the first year of life. If the baby is not cyanotic then it is sometimes referred to as a "pink tet."
2. Other symptoms include a heart murmur which may range from almost imperceptible to very loud, difficulty in feeding, failure to gain weight, retarded growth and physical development, dyspnea on exertion, clubbing of the fingers and toes, and polycythemia (Dark and concentrated blood).
3. Smaller children with tetralogy of Fallot may develop "tet spells." Tet spells are characterized by a sudden, marked increase in cyanosis followed by unconciousness and some times siezures ,may result in hypoxic brain injury and death. Older children will often squat during a tet spell, which increases systemic vascular resistance and allows for a temporary reversal of the shunt.
Surgical Repair
1. The Blalock-Taussig shunt procedure
when the blood flow to the lungs are so low that it causes danger to life of small kids (as definitive repair is high risk in very small underweight kids) or when the final repair is not feasible due to some technical reason the repair is devided in 2 stages. B.T Shunt is the first stage repair in which the tube made up of PTFE is connected between the aorta and the pulmonary artery. This shunting increases the blood flow in the lungs and hence the oxygenation increases ( though not 100%) and thus this gives the child to grow better for future corrective surgery and this also helps the smaller Pulmonary arteries to grow to normal size so as to be adequate for final surgery.
2. INTRA CARDIAC REPAIR
Total repair of tetralogy of Fallot cosists of
Prognosis
Untreated, tetralogy of Fallot rapidly results in progressive right ventricular hypertrophy due to the increased resistance on the right ventricle. This progresses to heart failure (dilated cardiomyopathy) which begins in the right heart and often leads to left heart failure. Actuarial survival for untreated tetralogy of Fallot is approximately 75% after the first year of life, 60% by four years, 30% by ten years, and 5% by forty years.
The procedure consists of approximately 5 % risk of death post operatively. This actually depends of time of repair, mostly patients appear for surgery very late and the disease is already advanced , but timely intervention (by the age of 1 to 3 yr.) results are pretty good.
Patients who have undergone total surgical repair of tetralogy of Fallot, have improved hemodynamics and often have good to excellent cardiac function after the operation with some to no exercise intolerance (New York Heart Association Class I-II). Surgical success and long-term outcome greatly depend on the particular anatomy of the patient and the surgeon's skill and experience with this type of repair.
Ninety percent of patients with total repair as infants develop a progressively leaky pulmonary valve later in adulthood. They require, therefore, follow up in specialized Adult Congenital Heart Disease centres. 55% are present.
TGA (Arterial Switch procedure)
What is dTGA ?
This is the disease in which the outflow onnection of the heart are wrongly connected . That means the Pulmonary artery (Artery which takes imimpure blood from the Rt side of the heart to lungs for purification) arises from Lt sided Chamber (LV). Whereas the Aorta (which supplies the pure blood from the Lt side heart chamber to whole body ) arises from the Rt sided chamber (RV).
Hence the pure blood circulates in lungs and the impure blood circulates in the whole body. If both the circulations donot mix blood via some hole in the heart , it may be a very serious condition and baby may not survive even for few weeks. But when hole is there both the pure and impure blood mix with each other and relatively less impure blood circulates in the body and gives some time for survival.
The arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA);
Timing
The arterial switch is ideally performed during the second week of life, before the left ventricle adjusts to the lower pulmonary pressure and is therefore unable to support thesystemic circulation.
In the event of sepsis or delayed diagnosis, a combination of pulmonary artery banding (PAB) and shunt construction may be used to increase the left ventricular mass sufficiently to make an arterial switch possible later in infancy.
Prognosis
The success of this procedure is largely dependent on the facilities available, the skill and experience of the surgeon, and the general health of the patient. Under preferable conditions, the intra-operative and post-operative success rate is 96% or more, with a comparable survival rate after 5 years.
How it is done
Post repair the patient is absolutely normal and lead a normal healthy life. As far as the life expectancy is concerned the post arterial switch patients have a normal and healthy life expectancy.
How is life after surgery?
Post repair the patient is absolutely normal and lead a normal healthy life. As far as the life expectancy is concerned the post arterial switch patients have a normal and healthy life expectancy.
Glenn
What do the Glenn and Fontan Procedures treat?
The Glenn and Fontan Procedures for Pediatric Patients
The Glenn and Fontan procedures are done to redirect blood flow. The procedures are done because one of the two ventricles cannot pump blood effectively. It may be weak, small or missing altogether.
The Glenn and Fontan allow blood to be routed directly to the lungs, leaving the ventricle that is able to work well to pump blood to the body.
What are the Glenn and Fontan Procedures?
What Should the Glenn and Fontan Procedures do?
After both of the Glenn and Fontan procedures are done, oxygen–poor blood from the body can travel to the lungs for oxygen. In cases where the left ventricle is missing or too small to pump blood, surgeons use these procedures to bypass the right side of the heart and send oxygen–poor blood directly to the lungs. The right ventricle may then be used as the heart’s main pumping chamber, sending oxygen–rich blood to the body.
Contraindications
After Fontan, blood must flow through the lungs without being pumped by the heart. Therefore children with high pulmonary vascular resistance may not tolerate a Fontan procedure. Often, cardiac catheterization is performed to check the resistance before proceeding with the surgery. This is also the reason a Fontan procedure cannot be done immediately after birth; the pulmonary vascular resistance is high in utero and takes months to drop.
The Fontan is usually done as a two staged repair.
The first stage, also called a Bidirectional Glenn procedure , involves redirecting oxygen-poor blood from the top of the body to the lungs. That is, the pulmonary arteries are disconnected from their existing blood supply (e.g. a shunt created during a Norwood procedure, a patent ductus arteriosus, etc.). The superior vena cava (SVC), which carries blood returning from the upper body, is disconnected from the heart and instead redirected into the pulmonary arteries. The inferior vena cava (IVC), which carries blood returning from the lower body, continues to connect to the heart.
At this point, patients are no longer in that delicate balance, and the single ventricle is doing much less work. They usually can grow adequately and are less fragile. However, they still have marked hypoxia (because of the IVC blood that is not fed into the lungs to be oxygenated). Therefore, most patients are referred for another surgery.
The second stage, also called Fontan completion, involves redirecting the blood from the IVC to the lungs as well. At this point, the oxygen-poor blood from upper and lower body flows through the lungs without being pumped (driven only by the pressure that builds up in the veins). This corrects the hypoxia and leaves the single ventricle responsible only for supplying blood to the body.
Approach
The Fontan is usually done as a two staged repair.
The first stage, also called a Bidirectional Glenn procedure , involves redirecting oxygen-poor blood from the top of the body to the lungs. That is, the pulmonary arteries are disconnected from their existing blood supply (e.g. a shunt created during a Norwood procedure, a patent ductus arteriosus, etc.). The superior vena cava (SVC), which carries blood returning from the upper body, is disconnected from the heart and instead redirected into the pulmonary arteries. The inferior vena cava (IVC), which carries blood returning from the lower body, continues to connect to the heart.
At this point, patients are no longer in that delicate balance, and the single ventricle is doing much less work. They usually can grow adequately and are less fragile. However, they still have marked hypoxia (because of the IVC blood that is not fed into the lungs to be oxygenated). Therefore, most patients are referred for another surgery.
The second stage, also called Fontan completion, involves redirecting the blood from the IVC to the lungs as well. At this point, the oxygen-poor blood from upper and lower body flows through the lungs without being pumped (driven only by the pressure that builds up in the veins). This corrects the hypoxia and leaves the single ventricle responsible only for supplying blood to the body.
Post-operative complications
In the short term, children can have trouble with pleural effusions, fluid building up around the lungs. This can require a longer stay in the hospital for drainage with chest tubes.
In the long term, children can have trouble with atrial flutter and atrial fibrillation because of scarring in the atrium, especially if the connection of the IVC to pulmonary arteries involved an intracardiac baffle (instead of an extracardiac conduit).
There are other long-term risks, includingprotein-losing enteropathy and chronic renal insufficiency, although understanding of these risks is still incomplete.
The Fontan procedure is palliative, not curative. But in many cases it can result in normal or near-normal growth, development, exercise tolerance, and good quality of life. In 20% - 30% cases, patients will eventually require heart transplantation.
MICS (Minimally Invasive Heart Surgery) Key Hole Heart Surgery
Minimally invasive heart surgery (also called keyhole surgery) is when a conventional operation is performed on or inside the heart using small incisions. The surgeon mostly uses specialized instruments.
Who Is a Candidate for Minimally Invasive or Robotic Surgery?
There are many ways to reach the heart for surgery. Surgeons always try to use the smallest incision to provide the safest but cosmetically successful surgery.
Your surgeon will decide the best approach for you based on several factors, including the type of heart disease you have and how severe it is; your age, medical history, and lifestyle; and results of tests done before surgery.
Benefits of Minimally Invasive Surgical Techniques
1) First and foremost is the fact that breast bone is either not cut or partially cut. This has several advantages in reducing pain, retaining function and having a positive effect on breathing. Unlike traditional heart surgery return to normal life including driving or other activities is not disrupted and can be started almost immediately.
2) Second, blood loss is almost negligible eliminating blood transfusion in most and eliminating blood borne infection.
3) Third, all infections are reduced whether it be wound infections or post surgical lung infection. This makes the procedure ideal in diabetics and older patients who have poor resistance to infection.
4) Fourth, the incision is so cosmetic and measures just 2 – 3 inches that it's practically impossible to tell that a heart operation has been done.
All these benefits put together make for ultra short hospitalization and recovery. The best part is that all the blocks irrespective of their location in the heart can be bypassed in a safe and predictable manner.
Traditional Heart Surgery
Traditional heart surgery uses an incision through the middle of your chest, through the breast bone. The incision is about 5 to 6 inches long.
This is the safest and most commonly used incision for patients who need complicated heart surgeries, reoperations, multiple coronary artery bypass procedures or complex aorta procedures.
Types of Minimally Invasive Heart Surgeries
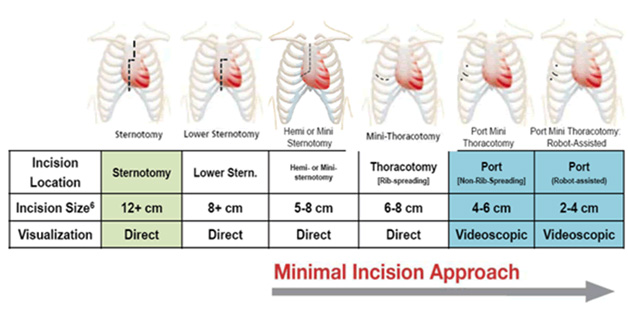
The first surgeries of this type were mitral and aortic valve surgeries. Now, a wide range of procedures can be done using minimally invasive techniques to help make recovery faster and more comfortable. Sometimes, minimally invasive surgery includes a partial sternotomy. This involves cutting through part of the breast bone. When possible, the surgeon can avoid cutting the breast bone and, instead, make one or more small incisions through the muscles between the ribs. This technique is called a mini-thoracotomy.
Types of Incisions Used in Minimally Invasive Heart Surgery
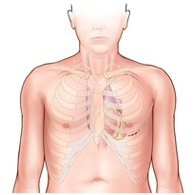
Partial Sternotomy - through part of the breast bone A 3- to 4-inch long incision is made through the sternum, and the breast bone is separated in that area so the surgeon can see the part of the heart that needs surgery.
Lower partial sternotomy: Used for the mitral valve, tricuspid valve, epicardial lead placement, atrial septal defect (ASD), patent foramen ovale (PFO), myxoma, and aortic valve surgeries.
Upper partial stgernotomy: Used for ascending aorta, aortic valve, mitral valve, tricuspid valve, two valves,transaortic TAVR, ASD, PFO, myxoma and fibroblastoma surgeries.
Mini-thoracotomy
The surgeon avoids cutting through the breastbone and, instead, cuts into muscles between the ribs to reach the heart.
Used for mitral valve, tricuspid valve, ASD, PFO, myxoma surgeries.
Used for aortic valve, transaortic TAVR and transaortic TEVAR surgeries.
Used for minimally invasive direct coronary artery bypass (MIDCAB), transapical TAVR, transapical TEVAR, and epicardial lead placement surgeries.
Recovery
If you have minimally invasive surgery, you will probably be able to go home 2 to 5 days after surgery. Your healthcare team will follow you closely while you are in the hospital and help you recover as quickly as possible. When you are ready to leave the hospital, you will get instructions on your recovery and return to work, including guidelines for activity, driving, incision care and diet.
Healthy Living
To keep your heart healthy after surgery, it is important to make lifestyle changes and take your medications as prescribed. Heart-healthy lifestyle changes that are important to your recovery include: